Stress and the Activity Based Stress Reduction Program (ABSR)
Background and Phenomena of the Stress Response and a Harmonisation with Exercises
Harald Haas
Last update: 06.04.2022
Traumatic Stress Response: Sequence of the Trauma Reaction - Comorbidities of Post-Traumatic Stress Disorder
If we look at the internal and external, subjective and objective symptomatology that occurs in trauma, an initially incomprehensible or life-threatening, frightening situation takes place. Followed by a response of freezing, immobility and cooling (in terms of the circulation, a centralization). This reaction is accompanied consciously by dissociation, confusion or a powerlessness (in fear of death) to do anything. Overcoming this state is only possible if an impulse of hatred, anger or an "escape impulse" can occur. This, however, only becomes possible when there is a physiological circulatory reaction, a flow of blood to the periphery. Outwardly this leads to blushing and is accompanied by a sense of shame or panic. The shame produces feelings of guilt, often accompanied by the experience of being ashamed of what has happened or even a feeling of guilt leading to an assumption of responsibility for the event by the "trauma victim" that is usually not justified.
In the long term, the stages of the trauma reaction process just mentioned can lead to a fixation of individual aspects. As an example, dissociation may develop into a dissociative disorder through repeated triggers, or the fear of death produce a persistent avoidance attitude to the point of agoraphobia. In the long term the development of shame and guilt may manifest in a depressive disorder or in avoidance leading to compulsive thoughts or actions. The reaction of hatred and anger can trigger an anti-social disorder or a general tendency to violent behavior.
In summary, the aspects just mentioned may be presented as in the overview below:
- fright - freezing – dissociation, (fear of death) - powerlessness
- → hate – anger (reaction)
- → shame - panic – guilt (assuming responsibility)
- → illnesses - long-term consequences - post-traumatic stress disorder with:
- Dissociative disorder, agoraphobia
- Propensity to violence
- Anxiety - Depression due to obsessive thoughts and compulsive actions.
Strangely enough, it may be observed that patients do not notice the dissociation, but immediately react with panic to a trigger situation. This may be understood by the fact that in the stress reaction, the powerlessness associated with dissociation is much more unpleasant than panic, as one cannot react to and free oneself from an inappropriate (1).
Further references to a spiritual-scientific differentiation of fear and post-traumatic symptomatology can be found by the author of this abstract in (2).
The history of trauma diagnosis
The study of traumatic memories began with the neurologist Jean-Martin Charcot (1825 -1893), the "father of neurology," who, at the Clinic Salpetriere in Paris, treated mental suffering according to the concept of "hysterical phenomena" which included paralysis, convulsions, fainting and emotional outbursts. His student Pierre Janet (1859 -1947) wrote the essay "L'automatisme psychologique" in 1889, where the clinical picture of today's post-traumatic stress disorder was described for the first time (3). The doctor and Depth-psychologist Sigmund Freud (1856 – 1925), who in his first publication together with Josef Breuer (1842 – 1925) in Vienna (4) had still referred to the trauma hypothesis of mental illness, later saw inner conflicts as the cause and thus denied the external event, the traumatization. Rudolf Steiner (1861 – 1925) experienced the development of psychoanalysis quite closely as a tutor of the Specht family in Vienna, where Josef Breuer was the family doctor.
According to Gregor Halser (5) disease frequencies of 0.5 % were found for trauma disorders in soldiers in WW1 and 2 % in WW2. "War injuries" which were considered to be hysterical neuroses.
I find this information regarding the 2nd World War very questionable. My own observations regarding the 2nd World War reveal that in the long run, in Germany, not only in soldiers, but also in the general population, the most frequent diagnosis of post-traumatic illnesses was called "vegetative dystonia" (diffuse complaints with no organic cause), which was very common. This is also mentioned in the book “Kriegskinder und Kriegsenkel” by Luise Reddemann (6). This "epidemic and collective suffering" in Germany led to a social processing by means of a pronounced "spa business" (with many spas all over the country and treatments covered by the general health insurance), quite in contrast, for example, to Switzerland, where the spa system never existed in this form. For some years now, the term "vegetative dystonia" has also been abandoned in Germany. Hasler further states that in the US military hospitals a diagnosis was needed for the treatment and possible retirement of traumatized Korean and Vietnam war veterans. This was no longer secured by the adoption of the European diagnosis system (ICD) incorporated into the Diagnostic and Statistical Manual of Mental Disorders (DSM), in terms of the psychiatrist Emil Kraepelin (1856 – 1925), in circa 1974. Therefore, the diagnosis "Post Traumatic Stress Disorder (PTSD)" was defined in the USA to secure this for the soldiers. Later, the diagnosis was applied primarily to sexual abuse and similarly serious experiences.
According to Hasler, the problem with this trauma concept based on empirical studies, is that 80% of people experience trauma, but only 20 to 60% suffer from acute trauma or trauma sequelae afterwards. Therefore, in ICD- 9 and 10, the recognized causes of a “Post-Traumatic Stress Disorder” were strongly limited to life-threatening events. In the current American version of DSM IV to DSM V the diagnosis is again broadened, especially in children up to 6 years of age. Further research, according to Hasler, showed that among U.S. military personnel, for example, the rate of suicide among war veterans was no greater than that among personnel who were not deployed to war. In the Iraq War, moreover, 31% of U.S. soldiers but only 2% of British soldiers developed PTSD, raising the question of other causes. Individual soldiers criticized the research for focusing on war situations alone and not on complex social difficulties.
In comparison, after the Fukushima disaster, those affected initially showed typical brain changes which then disappeared. The difficulty lies in the concept of PTSD, which focuses only on individual events, but not on complex psychosocial causal relationships and does not also take into account questions of resilience that could prevent a disease.
Only after the experiences in the military and war context did it become clear in the 1990's that especially sexualized violence presents a risk for the development of a complex post-traumatic stress disorder.
As an alternative to the "classic PTSD" the DSM -V provides the diagnosis Disorder of extreme stress not otherwise specified (DESNOS), which allows for complex manifestations with comorbidity and causal connections, which studies confirm are present in 40% to 60% of PTSD. For the ICD-11 of the World Health Organization (WHO), the recognition of the "Complex Posttraumatic Stress Disorder" has as of 2022 been achieved. Here a special manifestation with affective problems, negative self-image, relationship disorders, somatization and aggression with self-injury, is to be considered (7). In summary, it is clear that war experiences, in addition to individual psychological or physical violence, especially in the sexualized form, are among the most common factors causing trauma.
Own experiences of trauma-triggering causes
In my own practice, the "trauma consequence reaction" and comorbidities are not only manifested in individual death-threatening experiences or, as confirmed in the DSM V for children, in the experience of such by important attachment figures. Especially in highly sensitive people, everyday disregard or extreme religious or scientific doctrines in their environment can cause a "trauma-induced suffering". In addition, the above-mentioned poor social and economic conditions, which may lead to a violent mood and strong emotionality in the family, can also cause these reactions, or increase the suffering. It is well known that a mood of "high expressed emotion" in the family also favors this mental suffering (e.g., also in schizophrenic disorders). Peter A. Levine and Maggie Kline (8) also point out that even "normal" medical interventions in childhood can lead to trauma sequelae.
As a special cause of trauma, which has not been discussed much so far, the "clerical abuse" in the religious and social sphere should be mentioned. Pastoral abuse of power with dependence or brainwashing in the political realm, for example in communist systems, is meant (9). Except for extreme forms, such as so-called ritual abuse, this trauma dynamic is still little known.
Conclusion and psychodynamic treatment
Does the above mean that "everything is trauma"? This must be decisively denied, as a variety of psychodynamic and resilience aspects that may influence a trauma disorder also play a role. Coping with borderline experiences as a resilience factor is essential for the risk of developing a disorder. A central moment in developmental trauma is, which mental beliefs had to be acquired internally as protection in childhood or were adopted by the environment. This remains present in later life as introjects (according to Carl-Gustav Jung ( - )) or "negative beliefs". According to Luise Reddeman (10), an essential part of therapy is how to deal with these imprints, which have led to avoidance behavior regarding situations and relationships in life, in a healing and transforming way. According to her conviction this means, in general, with the exception of the so-called "monotraumas", the processing and transformation of introjects is preferable to trauma confrontation.
The approach of the Activity-Based Stress Reduction Program (ABSR)
Returning to the phenomena of the traumatic stress reaction, we find dissociation and shame increasing to panic as polarities.
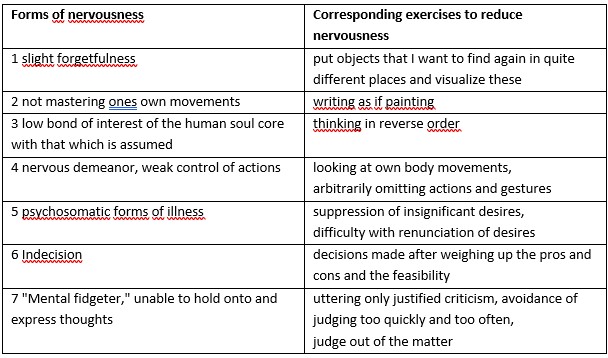
In the lectures Rudolf Steiner gave on the subject of psychoanalysis in 1917 (11) in Basel, a similar polarity is described. Steiner explained here, on the basis of the drawing below, the phenomena which are stated and treated by psychoanalysis as "nervous diseases". He describes these to be the "unjustified collapse", and as a "tumbling into each other" of the soul activities of thinking, feeling and willing, due to a weakened activity of the ego, which would correspond to the tendency to shame and panic (left side of the drawing). On the other side (right side of the drawing), there are pathologies that can be summarized under the concept of "dissociation", where the I is unable to hold the soul activities together.
If we look at the ABSR themes and exercises with this approach, as they appear on the following diagram, it becomes clear that the first three exercise areas aim to strengthen memory, the ability to act and the overview of consciousness, which is weakened or eliminated in dissociation and agoraphobia. The last three exercise areas support the Ego when at the mercy of compulsive behaviors, in improving the ability to make decisions and in getting lost in prejudices, which is typical of neurotic disorders with shame. The fourth exercise aspect is in the center and corresponds to the control of the actions on both sides of the deviation from the "center", where ideally the soul activities are held and ordered by the ego.
Overview of the therapy program
From the principles of these exercise approaches in relation to the polarities of the stress reaction, with the tendencies to dissociation and shame/panic with the comorbidities listed above, it can become clear that in the ABSR program help can be given for the one-sided pathological tendencies. In particular, the free ego decision and activity of the person is thus strengthened. This is further supported by the appropriate physical exercises of eurythmy, or eurythmy therapy.
Bibliography
- Reddemann L, Dehner-Rau C. Trauma verstehen, bearbeiten, überwinden: Ein Übungsbuch für Körper und Seele. 6. Aufl. Stuttgart: Trias Verlag; 2020.
- Steiner R. Self-Doubt: Depression, Anxiety Disorders, Panic, and Fear. Introduced and commented by Harald Haas. Forest Row: Rudolf Steiner Press; 2018.
- Levine, PA. Trauma und Gedächtnis. Die Spuren unserer Erinnerung in Körper und Gehirn. 3. Aufl. München: Kösel Verlag; 2020.
- Freud S, Breuer J. Studien über Hysterie (1895). Hofenberg; 2021.
- Hasler G. Resilienz: Der Wir-Faktor. Gemeinsam Stress und Ängste überwinden. 3. Aufl. Stuttgart: Schattauer; 2020.
- Reddemann L. Kriegskinder und Kriegsenkel in der Psychotherapie. 4. Aufl. Stuttgart: Klett-Cotta; 2017.
- Reddemann L, Wöller W. Komplexe Posttraumatische Belastungsstörung. 2. Aufl. Göttingen: Hogrefe; 2017.
- Levine PA, Kline M. Verwundete Kinderseelen heilen. Wie Kinder und Jugendliche traumatische Erlebnisse überwinden können. 13. Aufl. München: Kösel Verlag; 2005.
- Tempelmann I. Geistlicher Missbrauch. Auswege aus frommer Gewalt. Ein Handbuch für Betroffene und Berater. 3. Aufl. SCM R. Brockhaus; 2012.
- Reddemann L. Psychodynamisch Imaginative Traumatherapie: PITT®. Das Manual. Ein resilienzorientierter Ansatz in der Psychotraumatologie. 10. Aufl. Stuttgart: Klett-Cotta; 2020.
- Steiner R. Zwei Vorträge über Psychoanalyse. In: Individuelle Geistwesen und ihr Wirken in der Seele des Menschen. GA 178. 4. Aufl. Dornach: Rudolf Steiner Verlag; 1992.